What is Risperidone? Risperidone uses!
Risperidone belongs to a group of medication called antipsychotic (second generation). It works by balancing the levels of dopamine and serotonin in your brain, substances that help regulate mood, behaviors, and thoughts.
Antipsychotic medications can be used to treat several kinds of mental health conditions.
Risperidone used to treat schizophrenia symptoms. It is also used to treat mania and mixed symptoms in adults, adolescents, and children aged 10 and up who have bipolar disorder (manic depressive disorder; a disease that causes episodes of depression, episodes of mania, and other abnormal moods). The medication is also used to treat a variety of behavioral issues, including self-injury, and mood swings. It functions by altering the brain’s activity of certain natural substances.
Risperidone indications:
- Schizophrenia
- Mania
- Bipolar disorder
- Aggressiveness
Risperidone uses in other psychotics’ symptoms:
Positive Symptoms:
- Hallucinations
- Delusions
- Hostility
- Thought disturbances
Negative Symptoms:
- Blunted effect
- Emotional & social withdrawal
- Poverty of speech
Risperidone Dosage:
Risperidone tablets may be given in 1 or 2 divided doses daily. The usual and initial dose of risperidone tablets are 2mg and the usual maintenance doses of risperidone tablets are 4mg to 8mg daily.
Risperidone side effects:
The more common side effects of risperidone can include:
- nausea
- vomiting
- diarrhea
- constipation
- heartburn
- dry mouth
- increased saliva
- increased appetite
- weight gain
- stomach pain
- anxiety
- agitation
- restlessness
- difficulty falling asleep or staying asleep
- breast enlargement or discharge
- late or missed menstrual periods
- decreased sexual ability
- blurred vision
- back, muscle, or joint pain
- dry or discolored skin
- difficulty urinating
- dizziness, feeling unsteady,
- Having trouble keeping your balance
Risperidone and Pregnancy:
Research in animals has shown negative effects to the fetus when the mother takes the drug. However, there haven’t been enough studies done in humans to be certain how the drug might affect a fetus.
Newborn babies born to mothers taking this drug may have withdrawal symptoms.
These symptoms may include:
- restlessness
- limpness
- stiffness
- sleepiness
- breathing problems
Some newborns recover within hours or days without treatment, but others may need to be hospitalized.
Talk with your doctor if you’re pregnant or planning to become pregnant. And if you become pregnant while taking this drug, call your doctor. This drug should only be used if the potential benefit justifies the potential risk.
Risperidone and Breastfeeding:

Risperidone may pass into breast milk and may cause side effects in a child who is breastfed. Take advice from your doctor. You may need to decide whether to stop breastfeeding or stop taking this medication.
Warnings and Precautions:
Risperidone should be used with caution in patients with known cardiovascular disease (e.g. heart failure, myocardial infection, conduction abnormalities, hypovolemia, cerebrovasclar disease), and the dose should be gradually titrated as recommended. A dose reduction should be considered if hypotension occurs. It is recommended to have both the starting dose and the subsequent dose increments in geriatric patients and in patients with renal or liver insufficiency. Caution is also due to prescribing Risperidone to patients with Parkinson’s disease since, theoretically, it might cause a deterioration of the disease. Classical neruoleptics are known to lover the seizure threshold. Caution is recommended when treating patients with epilepsy. Patients may be advised to refrain from excessive eating in view of the possibility of weight gain.
Mechanism of action:
Though its precise mechanism of action is not fully understood, current focus is on the ability of risperidone to inhibit the D2 dopaminergic receptors and 5-HT2A serotonergic receptors in the brain. Schizophrenia is thought to result from an excess of dopaminergic D2 and serotonergic 5-HT2A activity, resulting in overactivity of central mesolimbic pathways and mesocortical pathways, respectively.
D2 dopaminergic receptors are transiently inhibited by risperidone, reducing dopaminergic neurotransmission, therefore decreasing positive symptoms of schizophrenia, such as delusions and hallucinations. Risperidone binds transiently and with loose affinity to the dopaminergic D2 receptor, with ideal receptor occupancy of 60-70% for optimal effect. Rapid dissociation of risperidone from the D2 receptors contributes to decreased risk of extrapyramidal symptoms (EPS), which occur with permanent and high occupancy blockade of D2 dopaminergic receptors. Low-affinity binding and rapid dissociation from the D2 receptor distinguish risperidone from the traditional antipsychotic drugs. A higher occupancy rate of D2 receptors is said to increase the risk of extrapyramidal symptoms and is therefore to be avoided.
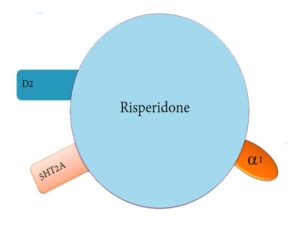
Increased serotonergic mesocortical activity in schizophrenia results in negative symptoms, such as depression and decreased motivation. The high-affinity binding of risperidone to 5-HT2A receptors leads to a decrease in serotonergic activity. In addition, 5-HT2A receptor blockade results in decreased risk of extrapyramidal symptoms, likely by increasing dopamine release from the frontal cortex, and not the nigrostriatal tract. Dopamine level is therefore not completely inhibited. Through the above mechanisms, both serotonergic and D2 blockade by risperidone are thought to synergistically work to decrease the risk of extrapyramidal symptoms.
Risperidone has also been said to be an antagonist of alpha-1 (α1), alpha-2 (α2), and histamine (H1) receptors. Blockade of these receptors is thought to improve symptoms of schizophrenia, however the exact mechanism of action on these receptors is not fully understood at this time.